20 Scenes From HIMSS 2009

The annual Healthcare Information and Management Systems Society (HIMSS) conference is one of the largest health-care IT gatherings in the world. This year's meeting, held April 4-8, brought upward of 27,000 people to McCormick Place in Chicago, hoping to get a better handle on topics that, thanks to technology advances and the federal stimulus, are getting hotter by the minute. Take a spin through HIMSS keynotes, the show floor and Chicago itself, courtesy of Channelweb.
While attendees walking through multiple buildings and exhibit halls at sprawling McCormick Place got exhausted, HIMSS kept up a healthy buzz. There were sessions on everything from the health IT implications of the American Recovery and Reinvestment Act to the latest and greatest in electronic medical records (EMR) systems, picture archive and communications system (PACS) imaging, and health-care information networks.

In the HIMSS opening keynote, actor Dennis Quaid recounted what he called one of the most frightening times of his life: in November 2007, when his newborn twins received a thousands-times-greater dosage of the blood thinner Heparin than they should have during a stay at Cedars-Sinai Medical Center in Los Angeles.
The ostensible reason was 10-unit and 10,000-unit dosage bottles that looked almost identical, but the broad implication, Quaid said, was a "system failure:" a lack of oversight, technological or otherwise, that combined with human error made for a dangerous situation. Quaid pleaded with HIMSS attendees to get health-care IT to a point where overworked medical staff would have a "backup" in 21st century technology.

Before HIMSS proper got under way, the Nursing Informatics Symposium brought nurse leaders together to talk about how IT can optimize the nurse's role in the daily workflow of a health-care setting. From left to right: Aurelia Boyer, RN, MS, MBA, senior vice president and CIO, New York-Presbyterian Hospital & New York-Presbyterian Healthcare System; Nympha Meindel, CIO, Kingsbrook Jewish Medical Center; and Peggy White, RN, MN, National Project Director, C-HOBIC (The Canadian Health Outcomes for Better Information and Care).

Dr. John Halamka, CIO of Harvard Medical School and the CareGroup Health System, gave attendees a two-word response to how they should approach stimulus opportunities: "Implement now."
As Halamka explained in both his address and in a Channelweb interview before he arrived in Chicago, the stimulus funds available through the American Recovery and Reinvestment Act of 2009 haven't started to flow just yet.
The much-discussed term "meaningful use"--the standard by which health-care organizations will be judged on the effectiveness of their EMR and thus given incentive payments--has yet to be defined by the Department of Health and Human Services. But Halamka advised health-care organizations not to wait, saying that the Office of the National Coordinator (ONC) for Health Information Technology will have a "laserlike focus on quality and efficiency."

The soon-to-be-former National Coordinator for Health Information Technology, Dr. Robert Kolodner, got a standing ovation during a town hall meeting at HIMSS. Kolodner, who said he's retiring and will be succeeded in the ONC post by Dr. David Blumenthal, was asked if he could "define meaningful use," prompting a roar of laughter in the hall.
Speaking last year at Everything Channel's Healthcare IT Summit in San Diego, Kolodner suggested that 2008 would be remembered as the "tipping point year" for health-care IT.
U.S. Sen. Sheldon Whitehouse (D-RI) told attendees during the HIMSS welcome address that he made health-care reform the subject of the first three pieces of legislation he introduced since he took office in 2006. Whitehouse is known in health-care IT circles for, among other things, having founded the Rhode Island Quality Institute, a collaboration between government officials, payers and providers to encourage the adoption of e-prescribing and EMR.

Keynoter George Halvorson, chairman and CEO of Kaiser Foundation Health Plan and Kaiser Foundation Hospitals, said that the U.S.' health-care delivery model of fee-for-service payments generates $2.5 trillion worth of revenue but remains a model of inefficient "pieces of care."
"We need computers to get it done," Halvorson said, suggesting that systematic change, buoyed by IT, would rescue the health system from its inefficiencies. "Physicians don't have enough information to do their jobs right. Paper records are incomplete, inaccurate and inaccessible."
The HIMSS exhibit hall--spread out into two halls at McCormick with a walkway in between--featured more than 900 vendors, including, according to HIMSS, about 200 first-time exhibitors. Attendees got a look at new solutions from veteran health-care vendors like McKesson, Siemens and GE, and HP, Dell and Xerox, as well as a long list of upstart players all with a piece of the exploding health-care IT market in mind.

Former Federal Reserve Chairman Alan Greenspan told HIMSS attendees that the economy hadn't yet turned upward but that the stabilization of equity market--signs of which he said he was seeing--would be the best indicator of that turnaround.
Greenspan identified the global economic crisis, the retirement of baby boomers and the coming storm over how to support Medicare as the major issues facing the economy overall.
"I hope that one of the avenues by which we'll seriously confront and improve these issues is in health-care IT," Greenspan said. "There are so many avenues there."

Speaking after Greenspan's keynote, HIMSS President and CEO H. Stephen Lieber (pictured) asked Greenspan if he thought the same cycle of "boom and doom" seen during the lead-up and fall during the dot-com bust and the current economic crisis was bound to happen again.
"When we had an economy that had been doing very well--which indeed we had before the dot-coms and before the housing troubles--you would tend to get people who would ordinarily be cautious reaching out," Greenspan said. "It's not an issue of people being uninformed. The problem was and is that in these types of bubbles, risk is increasingly underpriced. You can't forecast when a bubble is going to burst. A financial crisis by definition is a discontinuity of asset prices from one period to the next, almost overnight. If you could anticipate that, people would take actions to offset it."

This being Chicago, the late-night party scene was alive and well at HIMSS throughout the week.
One of the hot spots--a party hosted by Dell, Allscripts and Intel--brought a terrific funk and R&B cover band to Chicago's House of Blues. No cameras were allowed inside, so you'll have to take our word for it that it was a grand ol' time.

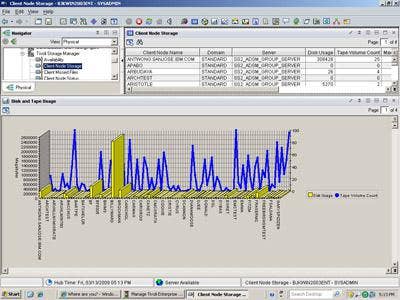
HIMSS-credentialed media were offered a chance to tour Chicago's Swedish Covenant Hospital. Its Stage 6 designation on HIMSS Analytics' Electronic Medical Record Adoption Model (EMRAM) puts it among the elite hospitals in the country from an IT integration perspective.
Only 25 organizations in the U.S. have been certified by HIMSS as Stage 6--meaning they not only have a functional electronic medical record and strong health-care IT infrastructure in place, but that they also serve as a model for health-care systems just beginning the process.
Mark Newton (pictured), Swedish Covenant's president and CEO, told reporters that a "dichotomy" existed in health-care IT.
"In some cases, we are significantly behind other industries, like the airlines and banks," he said. "And yet, we have all these immense diagnostic capabilities."

Before the tour of Swedish Covenant Hospital, CIO Karen Sheehan gave an overview of "thens" and "nows." For example, she said, before, nurse supervisors had to physically obtain a patient's charts from a Medical Records Office, and a health-care team relied on a patient's memory and language skills to understand the history and current situation.
Now, Sheehan said, an electronic medical record--Swedish Covenant uses Meditech software--means that there is no reliance on patient memory and language skills, test results are readily available, and doctors and nurses can have a full understanding of a patient's medical history and current situation before even meeting the patient.

Dr. Bruce McNulty, chairman of Swedish Covenant's Department of Emergency Medicine, demonstrated Swedish Covenant's computerized physician order entry (CPOE), which takes all the guesswork and cumbersomeness out of filing physician orders by electronically transmitting physician order information to a radiologist or phlebotomist.

Mimi Upp, Swedish Covenant's manager of Para-technical services, described how before, laboratory orders were sent to the lab and many labels were printed, prompting caretakers to sort labels, bring the correct labwork labels to each unit, find correct patients, draw blood and label it for the correct type of test.
Nowadays, Upp said, bar-code scanning technology means phlebotomists are alerted immediately when orders are filed, can scan patients to make sure they have the correct patient, and print bar-code labels right then and there for each patient. Bar-coded lab specimens are processed through an automated track system in Swedish Covenant's lab and, according to Upp and Clinical Laboratory Manager Susan Dawson, it takes an average of 18 minutes for a specimen to go through multiple lab tests.
Later in the tour, Dr. Bruce Silver, chairman of Swedish Covenant's Department of Radiology and Nuclear Medicine, and Joanne Hardt, assistant PACS administrator, demonstrated how advanced PACS imaging means quick and error-free evaluation of scanned images on computer screens.
Before, Silver and Hardt said, the traditional way was to look at scans and paper films on lightboards, and the benchmark turnaround time for results was 24 hours. The current system at Swedish Covenant is fully digital, 100 percent filmless and means turnaround time for results can be as low as two minutes, with 90 percent of them completed, according to Silver, in less than 12 hours.
Ramesh Patel (right), Swedish Covenant's senior director of Pharmacy and Clinical Research Services, said that in the past, nurses and pharmacists would have to manually obtain medications from a medication locker and place them in bins to be brought to each unit. It was not a secure location, Patel said, and there were no safety checks to ensure the pharmacist loaded correct medications and nurses pulled correct medications.
The system is now entirely automated, Patel said. He and cardiac telemetry unit nurse Emerald Pajak (left), demonstrated how nurses need a bio-ID to access medications from the automated system, a Pyxis profile shows a patient name and only the meds that that patient is one, meds are automatically dispensed in the correct dosage, and the caregiver can access only what is dispensed. At the patient's bedside, caregivers scan bar codes on both the medicine bin and the patient to ensure the correct meds in the correct dosages.
"It's checks and balances," remarked Dr. Derek Kelly (not pictured), Swedish Covenant's chief medical informatics officer, chief medical officer and vice president for medical management.
Throughout Chicago--from O'Hare Airport to street signs, subway lightboards and billboards like this one--HIMSS advertising was everywhere. In fact, during the week of the show, only one other thing dominated Chicago advertising with similar gusto ...
... and that was Chicago's ongoing bid to host the 2016 Olympics. From flags outside McCormick Place (pictured), to radio sound bites from Mayor Richard M. Daley and a glut of newspaper and television ads, the push for "Chicago 2016" was everywhere.

OK, Chicago, we get it. Olympics in 2016. Good luck to ya!